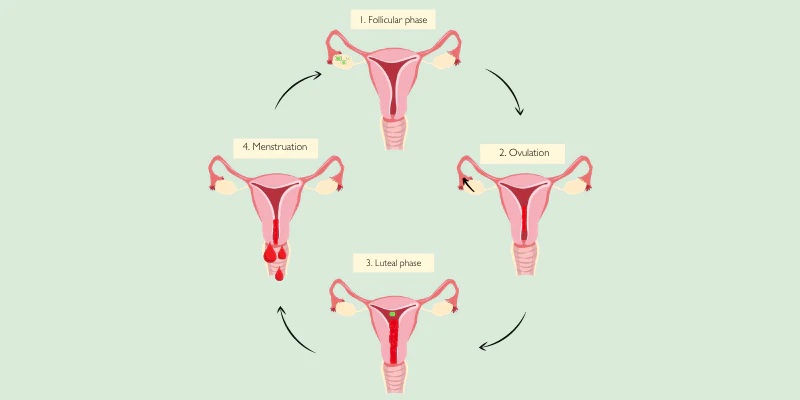
This is the second installment of our Period 101 series. You can read our first installment on healthy menstrual cycles here. Understanding the timeline of your menstrual cycle is important. We will try not to get too complex about the science behind it, but some of the details about the anatomy and physiology of the egg during the menstrual cycle may better help you to understand the changes in your vaginal mucosa and hormones during the different phases of your cycle.
-
- Phase 1 – Menstruation – (Days 1-7) You might think that your period is the last day of your cycle, but it is officially the beginning of your cycle. The first day of your period is the first day of your cycle. During your period, you are shedding the old uterine lining to start anew. This time signifies the lowest levels of estrogen and progesterone. The decline in progesterone and estrogen along with a drop in serotonin and a peak in inflammatory chemicals are responsible for the signs and symptoms that come in the days leading up to and the early days of our period.
-
- Phase 2 – The Follicular Phase – (Days 1 to 13) The start of your period is also the start of the follicular phase, named for the tiny ovum-containing follicles in your ovaries. One of these follicles become the dominant follicle, the ovum (egg) inside destined for release. Estrogen is dominant in this phase and continues to rise throughout. Testosterone also starts to rise, and you may feel bolder and more energized. Under the effects of estrogen, your uterine lining proliferates and gets ready for implantation should the egg get fertilized after ovulation.
-
- Phase 3 – Ovulation (Day 14 to 18) – This is the beginning of the luteal phase. The mature follicle opens, releasing the egg which travels down the fallopian tube to meet the sperm for fertilization. This egg can only be fertilized up to 24 hours after release. Sperm, however, can last in the fallopian tube for 3-5 days, so your fertile window is more like 5-6 days (ranging from about 5 days before ovulation to about 2 days after). During ovulation, Estrogen begins to peak, stimulating luteinizing hormone (LH). LH is what causes the follicle to release the egg.
- Phase 4 – Luteal phase (Day 14 to 28) – This phase typically lasts 14 days. The term luteal refers to the corpus luteum or yellow body which is the hollow on your ovary that is left after the egg was released from its follicle. Progesterone, which is produced by the corpus luteum, now takes over in this phase. Estrogen starts to increase towards its second, lesser peak of the cycle, along with increased testosterone. What happens in this phase depends on whether the egg is fertilized or not.
-
- 1. The egg is not fertilized. In the mid-part of this phase, estrogen and progesterone drop, causing the endometrium to shed. This leads to your period and the cycle starting over again.
- 2. The egg is fertilized. The fertilized egg travels through your fallopian tube to the uterine lining to implant and grow. The lining is essential for conception and it requires adequate progesterone and estrogen to optimize the lining’s thickness. The corpus luteum then continues to produce progesterone while the uterine lining grows to support the embryo as well as contributing to cervical thickness to protect against bacteria and additional sperm.
-
The luteal phase has two very different landscapes. In the first half, your energy is usually high and sex drive is ramped up. Your cervical mucus is plentiful and slippery. Your hormones are in a healthy flow, sleep is usually good, focus is high, and you are generally feeling good. Here the possibility for fertilization and embryo implantation is higher, particularly around ovulation. In the second half of the luteal phase (the week before your period) progesterone and estrogen start to decline and your cervical mucus will lessen and get thicker. In this form, the mucus is more limiting to sperm, making it harder for sperm to move toward the uterus which is now past its peak for embryo implantation.
So, to recap, we have started to review the basics of your period. In the first post Period 101, we discussed some period basics and characteristics of what a healthy period should look like. In this second installment, we talked about what an average cycle looks like and how it’s broken down.
In the next post, we’ll discuss the characteristics of cervical mucus and how to track your cycle. Stay tuned.
If you would like to read more about this in more detail, this information was taken from Hormone Intelligence. The Complete Guide to Calming Hormone Chaos and Restoring Your Body’s Natural Blueprint for Well-Being. (2021) by Dr. Aviva Romm, MD.
Written by Stephanie Muntzer, MPT, PYT, RYT200, CPI, SFMA, FMSc